
Robotic Process Automation (RPA) has emerged as a game-changing solution, offering unprecedented efficiency and accuracy in medical billing processes. By automating repetitive tasks, RPA technology streamlines operations to enhance accuracy, boost efficiency, and maximize revenue. Let’s dive into the benefits of RPA in the medical billing process.
Understanding RPA in Healthcare
Robotic Process Automation is a technology that uses software robots to automate routine, rule-based tasks traditionally performed by humans. In medical billing, RPA acts as a digital workforce that operates 24/7, processing claims, verifying insurance eligibility, and managing patient data with remarkable precision.
The Strategic Role of RPA in Medical Billing
RPA is crucial to the medical billing process by automating tasks such as claims posting, eligibility verification, and payment processing and posting. This technology integrates with existing systems to enhance efficiency, accuracy, and compliance.
Streamlined Operations
- Automated eligibility verification and benefits checking
- Real-time claim status monitoring
- Automated payment posting and reconciliation
- Intelligent denial management and appeals processing
Enhanced Accuracy
- Reduction in human error through automated validation
- Consistent compliance with healthcare regulations
- Standardized documentation and audit trails
- Automated updates for changing payer requirements
Accelerated Revenue Cycle
- Faster claims processing and submission
- Reduced days in accounts receivable
- Improved first-pass claim acceptance rates
- Enhanced cash flow management
Implementation Strategy for Maximum Efficiency
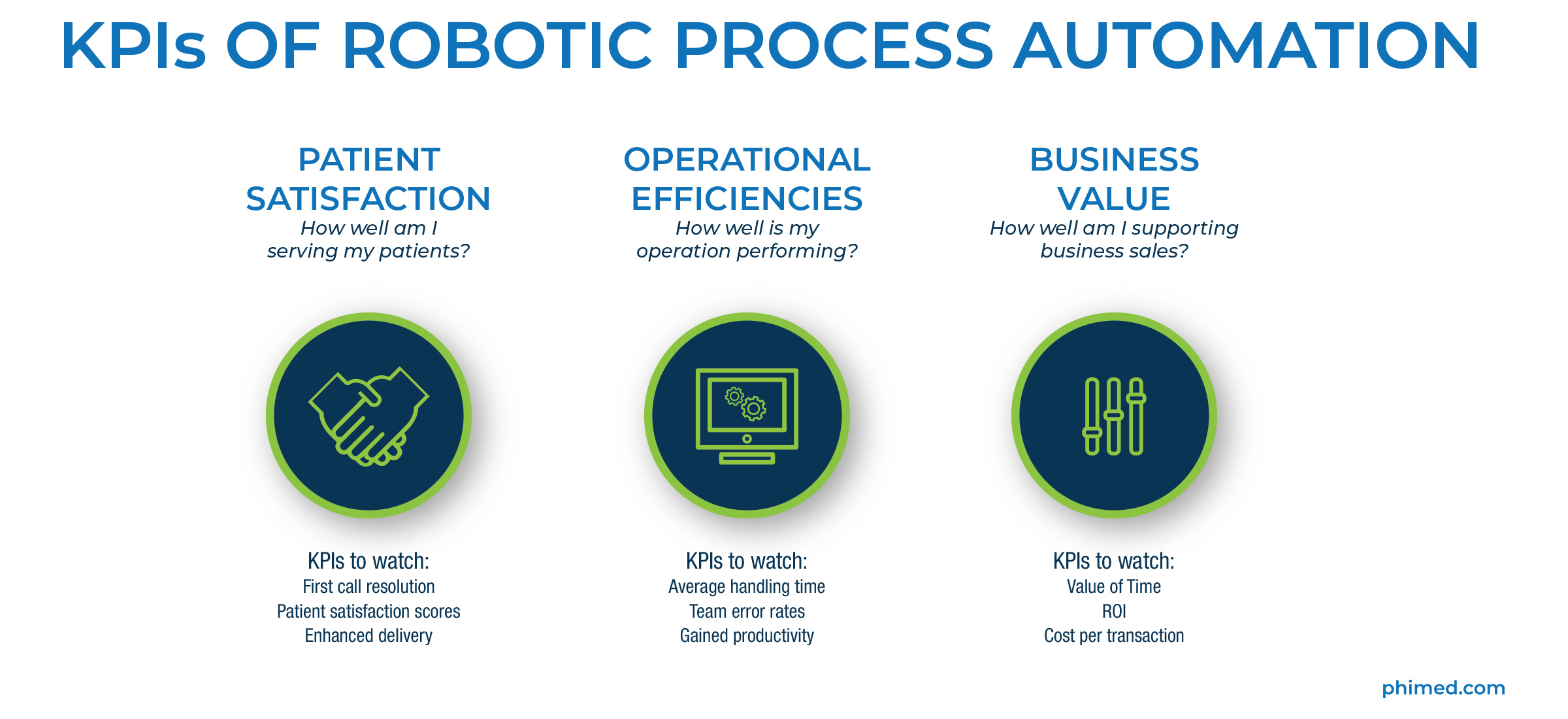
Effective RPA implementation begins with Process Assessment and Optimization. Healthcare providers should identify high-volume, repetitive tasks, map workflow bottlenecks, and prioritize automation opportunities. Setting clear KPIs ensures measurable success from the start.
Next is Technology Integration. PhyGeneSys integrates seamlessly with existing practice management systems, offering customized workflows, flexible implementation options, scalable solutions, and real-time analytics to optimize operations without disrupting current systems.
Finally, Cost Savings and ROI are quickly realized. Automation reduces manual labor and overtime costs, minimizes error-related expenses, and improves resource allocation, allowing staff to focus on more strategic, patient-focused activities.
Enhanced Patient Satisfaction
The implementation of RPA technology has transformed the patient experience in remarkable ways. Patients now experience significantly faster claim processing times, dramatically reducing the frustrating delays that often plague traditional billing systems. Through automated verification processes, patients receive more accurate billing statements the first time, eliminating the confusion and stress associated with billing errors. The system’s ability to manage automated patient communication ensures timely updates about claim status and payment requirements, keeping patients informed throughout the process.
Payment plan management has also been revolutionized through RPA, offering patients more flexible and accessible payment options with immediate processing and confirmation. Real-time eligibility verification means patients understand their coverage and financial responsibilities before receiving services, preventing unexpected bills and improving satisfaction. The streamlined prior authorization processes have significantly reduced treatment delays, allowing patients to receive care when they need it most.
Future Trends in Medical Billing RPA
The future of RPA in medical billing promises even more transformative innovations through artificial intelligence integration. Machine learning algorithms are being developed to further improve accuracy and predict potential claim denials before they occur. Natural language processing is revolutionizing documentation processes, making it possible to automatically extract and process relevant information from various medical documents with unprecedented accuracy. These advancements in intelligent automation are enabling more sophisticated decision-making capabilities that can handle increasingly complex billing scenarios.
Interoperability is evolving to new heights as RPA systems become more sophisticated. Modern solutions offer seamless integration between different healthcare systems, enabling real-time data synchronization that keeps all stakeholders informed and aligned. Enhanced reporting capabilities are providing deeper insights into billing processes, while advanced analytics tools are helping practices identify trends and opportunities for optimization that were previously invisible to human operators.
The scope of automation capabilities continues to expand, with RPA systems now managing increasingly complex workflows that once required significant human intervention. Advanced decision support systems are being integrated to handle nuanced billing scenarios, while automated compliance monitoring ensures adherence to ever-changing healthcare regulations. Predictive maintenance and optimization features are being developed to automatically identify and resolve potential issues before they impact billing operations, ensuring continuous improvement in processing efficiency and accuracy.
As healthcare continues to evolve, RPA technology stands at the forefront of medical billing innovation. By implementing robust RPA solutions, healthcare providers can significantly improve their revenue cycle management while reducing operational costs and enhancing patient satisfaction.
Schedule a Discovery Call today to learn more about PhyGeneSys and the implementation of RPA.





